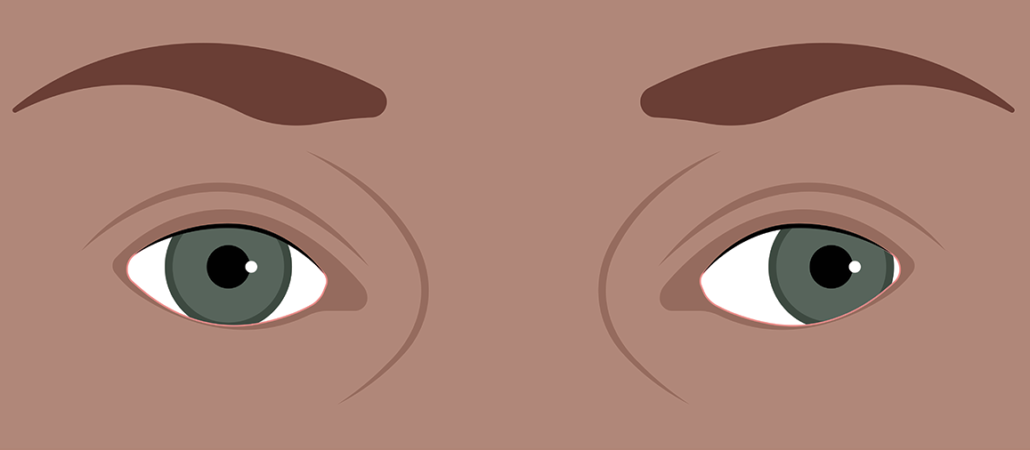
Exotropia typically develops in a progressive course but this progression can be very gradual. At first, the eyes rarely turn outward, such as when the patient is tired or sick. This is exophoria. Next, the eyes spontaneously deviate when the patient is more alert/awake. This is intermittent exotropia. Finally, the intermittent exotropia becomes increasingly frequent, and the eyes are constantly turned; this is constant exotropia.
As noted above, exotropia can progress slowly over time. Sometimes, there is no progression beyond the phoria or intermittent stages. In theory, it is better to operate on an intermittent exotropia because the binocular cells are still functioning and still have the capacity to keep the eyes aligned at least some of the time. In practice, many people who have had years of constant exotropia have their depth perception restored with surgery.
So, when is the best time to operate? There are three considerations: how often the strabismus occurs, whether it is causing visual symptoms, and whether it is causing self-esteem issues. These are very individual considerations and there is no “right” answer. The timing of surgery is always elective.
A few more things about exotropia: First, people who are myopic (near-sighted) and have an exotropia should wear their glasses all the time because this can help to limit the frequency of the exotropia. Second, there is a form of exotropia where eye exercises can help. If the eyes turn out more at near than when looking at something far away, this is convergence insufficiency (CI). With CI, specific eye exercises can be effective if performed properly. Convergence insufficiency is the only type of strabismus that has been demonstrated to respond to eye movement exercises.